The FDA’s Quality Management System Regulation (QMSR) replaces the legacy QSR and formally incorporates ISO 13485:2016 (and ISO 9000:2015 Clause 3 for terminology) by reference. The final rule was issued on February 2, 2024, with an effective date of February 2, 2026 and it arrives with a new, lifecycle‑focused inspection model that retires QSIT.
Why did FDA replace QSR with QMSR?
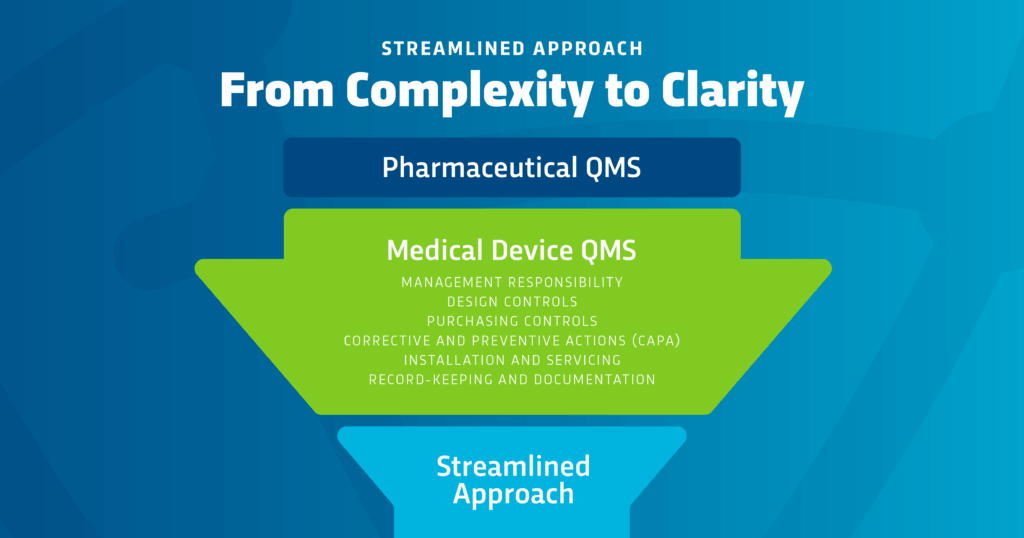
For nearly three decades, manufacturers managed a U.S. QSR that diverged from global practice, creating duplicate compliance burdens. QMSR harmonizes with ISO 13485, modernizes expectations, and preserves specific U.S. obligations where needed, improving clarity while reducing redundancy for firms marketing in multiple jurisdictions.
The headline changes you’ll notice
ISO 13485 becomes the backbone of U.S. device CGMPs
QMSR restructures Part 820 to function as an overlay on ISO 13485:2016 (and ISO 9000:2015 for definitions), while retaining targeted FDA additions to avoid conflicts with U.S. requirements (e.g., records and labeling/packaging clarifications).
New inspection model; QSIT is retired
On the effective date, FDA begins inspections under Compliance Program 7382.850 and discontinues QSIT. Expect risk‑based planning, integration of post-market and lifecycle data, and inspectors following issues across processes rather than auditing subsystems in isolation.
Analyses show FDA will organize inspections around six QMS Areas and cover four “Other Applicable FDA Requirements” (MDR, Corrections/Removals, Tracking, UDI), often starting with your risk management file as the roadmap.
Terminology alignment: DHF/DMR/DHR → ISO terms
QMSR sunsets QSR‑only terms in favor of ISO vocabulary:
- Design History File (DHF) → Design & Development File (DDF)
- Device Master Record (DMR) → Medical Device File (MDF)
- Design History Record (DHR) → Manufacturing Records/Records
FDA notes the content obligations remain under ISO clauses (especially 4.2 and 7.x) and retaining the old terms would be redundant and confusing.
Practical tip: You don’t have to rename every document, just ensure your files demonstrably meet ISO 13485 content and traceability, and keep a clear mapping for inspection.
Internal audits & management reviews are now fair game
Under QMSR and its new compliance program, industry observers and FDA‑facing legal analysts note that internal audits, supplier audits, and management review records are no longer categorically exempt. Treat them as inspection‑ready evidence.
MDSAP updates and new home
The MDSAP Audit Approach has been updated to Version 10 and is now hosted on MDSAP. Global, managed by Australia’s TGA, important for firms relying on MDSAP for global oversight alignment.
What doesn’t change—and where FDA adds clarity
QMSR supplements rather than displaces certain U.S. obligations. You should continue to reference UDI (21 CFR Part 830) and Medical Device Tracking (21 CFR Part 821) where ISO 13485’s text isn’t sufficiently specific for U.S. needs. FDA’s Part 820 overlay also emphasizes records and labeling/packaging controls to ensure U.S. expectations remain explicit.
Design controls under QMSR: clarifying Class I and risk
Class I exemptions: If your device was previously exempt from design controls, that status remains; QMSR doesn’t retroactively impose design controls on exempt devices. (Narrow exceptions for specific Class I products continue as before.)
Risk integration: Inspectors now begin with your risk management documentation and trace how risks drive design decisions, supplier oversight, production controls, and post-market actions reflecting the ISO 13485/ISO 14971 emphasis and the new compliance program’s lifecycle scope.
Inspections under CP 7382.850: what FDA evaluates now
FDA will test whether your QMS works as an integrated, risk‑driven whole:
- Risk‑based sampling guided by your risk files; investigators follow issues across functions.
- Lifecycle data integration (complaints, MDRs, recalls, servicing, supplier issues) feeding back into design/manufacturing changes.
- Six QMS Areas + four OAFRs (MDR, Corrections/Removals, Tracking, UDI) form the backbone of inspection scope.
Do I have to buy ISO 13485 now?
Because QMSR incorporates ISO 13485 by reference, firms need to control the standard as an external document inside their QMS, typically requiring purchase and version control (per ISO 13485 clause 4.2.4 on external documents).
If you’re already ISO 13485‑certified: the lift is manageable
Most of the effort is validating coverage of the Part 820 overlay and tightening traceability to U.S. obligations (MDR, UDI, tracking, labeling controls). Expect incremental updates for servicing/installation records and labeling release/reconciliation to match FDA clarity.
FAQs
Q: Does QMSR change Class I design control exemptions?
A: No. Devices previously exempt remain exempt (with the same narrow exceptions).
Q: Does ISO 13485 certification replace FDA inspections?
A: No. FDA still inspects under QMSR and CP 7382.850; certification helps, but it’s not a substitute.
Q: Do we have to rename DHF/DMR/DHR?
A: Not necessarily. Ensure your content satisfies ISO 13485, maintain a clear mapping, and be consistent in training and retrieval.
How Regulatory Compliance Associates Can Support Your QMSR Transition
The shift from QSR to QMSR is more than a terminology update, it’s a transformation in how quality systems are evaluated. With ISO 13485 as the legal backbone of Part 820 and a risk‑based, lifecycle inspection model replacing QSIT, the standard is clear: demonstrate real‑world system effectiveness.
Why partner with RCA now?
- QMSR Gap Assessment & Implementation Support—map current QSR systems to ISO 13485 + FDA overlay (records, labeling/packaging).
- SOP & Document Modernization—align MDF/D&D files and manufacturing records with inspection‑ready ISO/FDA expectations.
- Risk Management Integration—embed ISO 14971 across design, suppliers, production, and post-market—the first stop for investigators.
- Mock FDA Inspections (CP 7382.850)—train on the new lifecycle framework (risk‑based sampling; six QMS Areas + OAFRs).
- MDSAP Alignment—update readiness to MDSAP Audit Approach v10 (MDSAP.Global).
Ready to strengthen your quality system and prepare for QMSR?
Contact Regulatory Compliance Associates today to schedule a QMSR readiness review or request a customized support plan. Your next inspection will test how your system performs, not just what’s on paper.